The following article is from the Chinese Journal of Experimental Ophthalmology, the author consensus expert group
[Abstract] intense pulsed light (IPL) therapy is one of the physical therapies for meibomian gland dysfunction (MGD) and MGD related dry eyes. Recently, it has attracted more and more attention from clinicians. The principle of IPL in the treatment of MGD and its related dry eyes is to improve the microenvironment of meibomian gland and ocular surface, reduce the level of inflammatory factors in ocular surface tissue, improve tear film homeostasis and reduce the inflammation of eyelid margin by using the photothermal effect, thermal radiation effect, sterilization, anti-inflammatory, light regulation and restoration of local hypoxic environment of wide-spectrum incoherent light, To achieve the purpose of treating MGD and MGD related dry eyes and reducing the ocular symptoms and signs of ocular surface diseases. As a new treatment for MGD and related dry eyes in recent years, the clinical efficacy and safety of IPL have been gradually recognized. However, at present, due to the relative lack of clinical application practice of IPL, more types of products, more individual influencing factors of patients in the treatment process and the need for personalized selection of treatment parameters, the clinical indications, treatment parameter adjustment, treatment operation process, treatment timing and course of treatment of MGD related dry eyes treated with IPL There is no standardized guidance on the evaluation of curative effect and the determination of treatment plan. The consensus expert group on the clinical application of dry eye IPL has made extensive investigation and careful discussion, and formulated this consensus on the standardized operation process of IPL based on the application progress and action principle of IPL in Ophthalmology, so as to provide recommendations for the standardized clinical application of IPL and provide basis for the standardization of diagnosis and treatment mode of dry eye diagnosis and treatment centers in China.
Meibomian gland dysfunction (MGD) is a common chronic and diffuse eye disease characterized by abnormal meibomian gland function and structure. It can lead to obstruction of meibomian gland orifice, change of meibomian gland secretion or quantity, obstruction of discharge, change of tear film, and then cause eye irritation symptoms and ocular surface inflammatory reaction, Even serious dry eyes. In addition, the meibomian gland mainly secretes lipids, forming the lipid layer of tears, which can prevent the rapid evaporation of the tear water layer. Therefore, MGD often leads to the decline of tear film stability in patients, which is closely related to the occurrence and progress of dry eyes. It is reported that the prevalence of MGD in Asia is as high as 70% [1]. MGD is one of the common causes of hyperevaporation dry eye, which can lead to chronic inflammatory manifestations such as severe corneal lesions, foreign body sensation, burning sensation, pain, blurred vision, photophobia, tears and abnormal changes of mucosa and skin around the eyelid margin. Bacterial infection caused by long-term inflammation can further cause the destruction of meibomian gland and aggravate the condition of dry eye. The main causes and risk factors of MGD related dry eyes include blepharitis, mite infection, corneal contact lens wearing, long-term ametropia, use of electronic terminal products, dry environment, air pollution, lack of sex hormones, antidepressants, antihistamines, retinoic acid, Sjogren's syndrome and some systemic diseases. Due to various causes, complex inflammatory mechanism and repeated course of disease, Therefore, the treatment is difficult, which seriously affects the quality of work and life of patients, and brings considerable social and economic burden to the medical service system [2].
The main link of MGD dry eye treatment is to improve the structure and function of meibomian gland. At present, there are a variety of intervention measures for MGD treatment. The commonly used methods include oral or local application of antibiotics, glucocorticoids and anti-inflammatory drugs, supplement of nutrients, adjustment of life or work style and surgical treatment, but the long-term curative effect is not good [3-5]. In recent years, intense pulsed light (IPL) has been used in the treatment of MGD and has gradually attracted extensive attention of clinicians.
IPL is a broad-spectrum pulsed light with a wavelength of 500 ~ 2000 nm. Dermatology department mainly uses its selective photothermal principle as a common non-invasive and non laser skin rejuvenation treatment technology. The light energy released by IPL is preferentially absorbed by hemoglobin, melanin and water and converted into heat, resulting in coagulation and ablation of vascular tissue and destruction of melanin [6]. At the beginning of the 21st century, IPL was found to reduce the clinical symptoms and signs of MGD or MGD related ocular surface diseases when used in the lower eyelid cheek skin. In recent years, the research on IPL in the treatment of dry eye in China has gradually deepened and attracted extensive attention. At present, IPL has become one of the indispensable physical means for the treatment of dry eye in the construction of dry eye diagnosis and treatment center [4]. As a new clinical treatment of MGD and its related dry eyes, IPL treatment can significantly improve the symptoms of patients with MGD related dry eyes, reduce the related ocular surface evaluation indicators and improve the function of meibomian gland [7]. IPL can restore or reconstruct tear film function by reducing blepharal congestion and ocular surface inflammation, and its efficacy and safety have been confirmed [4,8-9].
In view of the pathogenesis of MGD related dry eye, 2017 TFOs dews II, the consensus of Chinese dry eye treatment experts in 2020 and recent new relevant studies have listed IPL as an important method of comprehensive treatment of dry eye [10-11]. IPL has the characteristics of non-invasive, relatively safe, rapid effect and positive curative effect. Therefore, it is increasingly widely used in clinical practice in China, However, at present, there is no unified standard for the clinical indications, treatment parameters, treatment process, operation methods and efficacy evaluation of IPL for dry eye treatment, which leads to some patients not reaching the ideal effect after treatment, which has an adverse impact on the clinical application and promotion of this technology, and is not conducive to the systematic evaluation of patients' treatment effect and the prevention and treatment of potential adverse reactions.
With the wide application of IPL in the treatment of MGD and its related dry eye methods in China, some non-standard application methods have attracted our attention. MGD and MGD related dry eye are common and frequently occurring diseases in China, and the prevalence is gradually increasing. The technology of IPL for MGD and MGD related dry eye is still in the stage of popularization and application. Standardizing the use of this technology to achieve the ideal treatment goal is still facing potential challenges. In order to standardize the clinical application of IPL therapy in the treatment of MGD and related dry eyes in China, the dry eye rehabilitation professional group of the visual rehabilitation Committee of China Rehabilitation Medical Association organized relevant researchers to investigate and discuss the research progress of IPL in the field of MGD and related dry eyes at home and abroad according to the clinical characteristics of MGD and related dry eyes in China and the technical characteristics of IPL equipment, The following consensus of Chinese experts on the clinical application of IPL ophthalmology is formulated to standardize the treatment methods and steps of clinicians using IPL for MGD related dry eyes.
1. Consensus making method
Relying on the dry eye rehabilitation professional group of the visual rehabilitation professional committee of the Chinese Rehabilitation Medical Association, an expert consensus expert group on the clinical application of dry eye IPL is established. The expert members participating in the consensus formulation must meet the following conditions: (1) members of the dry eye rehabilitation professional group of the visual rehabilitation professional committee of the Chinese Rehabilitation Medical Association; (2) More than 10 years of professional work related to the diagnosis and treatment of ocular surface diseases in China, with senior professional and technical titles; (3) Academic leaders in the diagnosis and treatment of ocular surface diseases in various regions of the country. Members of the consensus making group conducted in-depth investigation and Research on the general situation of IPL treatment of dry eye in China, collected and summarized the main problems in the application of this technology, and fully searched and reviewed the relevant literature at home and abroad (due to the lack of relevant research on IPL treatment of dry eye Technology, the evidence category and level of the research literature were not strictly evaluated), On the basis of carefully evaluating the clinical symptoms and pathological mechanism of related diseases, an expert discussion was held. At the same time, the main problems existing in the proposed IPL treatment of MGD and its related dry eye methods were repeatedly demonstrated, and a consensus was gradually reached on the standardization of related dry eye treatment and operation. After the formation of this consensus, the members of the expert consensus group were invited to modify it by email for many times, and finally the modification opinions were discussed through online meeting to form the final draft of the consensus. The consensus has gone through more than one year from its inception to its completion.
2. Working principle and development process of IPL
IPL is a kind of light emitted in pulse mode and belongs to non laser light source. It has the characteristics of wide spectrum range and high energy density. Its basic working principle is that the trigger applies high voltage to xenon to trigger xenon ionization. After charging for a long time through the energy storage capacitor, it is fully discharged in a very short time, causing xenon avalanche ionization in the lamp tube, Xenon converts the electric energy accumulated by charging in the form of high-intensity light radiation and releases it instantly. This discharge process is an optical pulse with an output wavelength of 400 ~ 1200 nm. Different cut-off filters can be used according to different indications to obtain the required wave band. The longer the wavelength, the deeper the tissue penetrated. IPL contains 1 ~ 3 sub pulses. The pulse width of sub pulses and the pulse delay between sub pulses can be adjusted, generally in milliseconds. The working principle of IPL is based on selective photopyrolysis. When the wavelength of incident light matches the inherent absorption peak of the target color base and the irradiation time exceeds the thermal relaxation time of the target color base, the target color base can be selectively destroyed to achieve the therapeutic effect. The target color base of IPL for MGD related dry eye treatment is hemoglobin. During the treatment process, light energy is absorbed by hemoglobin and converted into heat energy, which increases the temperature of target tissue and solidifies, so as to close the capillaries with abnormal expansion of palpebral margin [12]. IPL can also indirectly inhibit the release of inflammatory mediators in local tissues through various effects, so as to block the inflammatory cascade and improve dry eye symptoms [12]. IPL equipment was first used in clinic in 1994 and was approved by FDA for the treatment of dermatological diseases in 1995. After decades of development, the IPL equipment widely used in clinic has been updated to the fifth generation. Clinical research shows that a variety of pulse light equipment show good therapeutic effects on dry eyes.
3. Mechanism of IPL in the treatment of MGD and its related dry eyes
At present, clinical and basic research evidence shows that the principle of IPL in the treatment of MGD is not completely clear, which may include the following mechanisms: (1) selective photothermal effect. IPL can close the dilated capillaries of the palpebral margin through selective photothermal effect, and the occlusion of atypical erythema vessels can significantly reduce the secretion of inflammatory mediators, so as to remove a large number of inflammatory sources in the eyelid and meibomian gland [10]. (2) Thermal radiation effect after local application of IPL on the eyelid, it can emit thermal radiation effect on the meibomian gland and melt the eyelid fat of meibomian gland [12]. IPL has a fairly wide infrared wave frequency and is the heat source for thermal effect. It can act on the local eyelid tissue, increase the temperature in the local tissue and spread to the eyelid fat, soften and discharge it, dredge the meibomian gland duct, and restore and improve the ability to excrete eyelid fat in the blink of an eye [7]. (3) Reduce the microbial load of mites and Propionibacterium acnes on the palpebral margin. The heat generated by IPL can be higher than the appropriate temperature for the survival of mites, interfere with the survival environment of mites, induce coagulation and necrosis of proteins in mites, and block the cascade reaction of inflammation, so as to achieve the purpose of treating mite blepharitis [13-14]. The reducing effect of IPL on microbial load of eyelid skin can be used in the treatment of acne propionate blepharitis. (4) Anti inflammatory effect IPL can up regulate the expression of anti-inflammatory factors in local tissues, down regulate the expression of pro-inflammatory factors in tissues, inhibit the activation of matrix metalloproteinases and promote the balance of eyelid microenvironment; (5) Light regulation the light emitted by IPL can induce changes in tissue and cells at the gene and / or protein level. The photochemical cascade produced by IPL can stimulate meibomian gland cell mitochondria to increase the production of adenosine triphosphate, modify its output reactive oxygen species and change transcription factors [15]. Studies have found that IPL can change the activity of meibomian gland acinar cells through light regulation and alleviate the inflammatory response of glands and surrounding tissues [16]. (6) Restore the hypoxic environment of meibomian gland. Meibomian gland is a low oxygen consuming tissue. The hypoxic environment can promote the differentiation of meibomian gland epithelial cells and stimulate their secretory function. IPL treatment can restore the hypoxic environment of meibomian gland by closing abnormal dilated blood vessels [17].
4. Operation process and IPL parameters of MGD
At present, the IPL devices available in clinic are mainly represented by optimal pulse technology (OPT) and intensive regulated pulsed light (irpl), which can set different treatment parameters for patients with different indications and skin colors. The adjustable energy gradient is 10 ~ 16 J and the pulse width is 3.5 ~ 13 Ms, The pulse delay is 40 ~ 60 ms. According to Fitzpatrick's skin classification standard, the skin type of Chinese people belongs to type III ~ IV, and the filter is 590 nm (type IV skin) / 560 nm (type III skin). During IPL treatment, eye protection measures should be taken for patients, such as wearing appropriate eye masks to focus the light on the skin around the eyelids, and adjusting the irradiation energy, pulse width and pulse delay parameters by evaluating the patient's skin state, skin pigment and pain response during treatment. The operator can gradually increase the energy according to the patient's tolerance. If the treatment site is the upper eyelid, use low-energy parameters and prolong the pulse delay time. Before treatment, a test spot should be made on the patient's cheek to closely observe the skin reaction. Those with warm feeling or slight tingling feeling are normal treatment reactions.
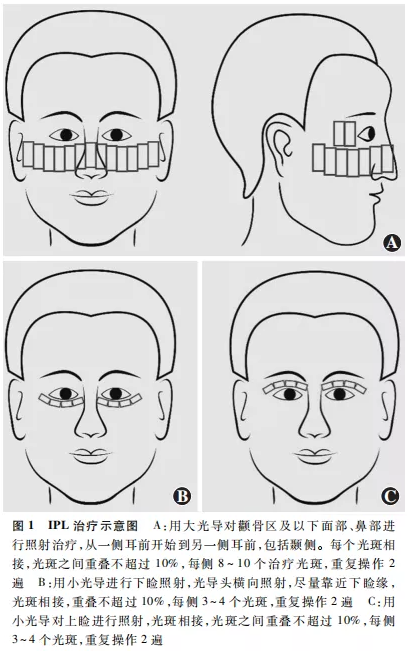
It is recommended that IPL be treated according to the following steps: (1) clean the face thoroughly and clean sunscreen, cream and foundation. (2) Eye protection: cover the patient's eyes with blackout eye patch or eye mask, and remind the patient to close their eyes in the whole process of treatment; If it is necessary to treat the upper eyelid area, a built-in eye shield should be considered to protect the inner eye tissue from radiation damage; (3) gel applied and tested all treatment areas evenly coated with photon therapy gel, with a thickness of about 2 mm; Put a test spot on one cheek to observe the skin reaction and ask the patient how they feel; (4) IPL irradiation will light the treatment head on the gel and start the light spot from the side of the patient's ear. It will be irradiated along the lower eyelid as close to the palpebral margin as possible. The face and nose of the zygomatic region and below can be treated until the other side of the ear. Each treatment spot shall be connected, and the overlapping part of the spot shall not exceed 10%. Complete operation twice. Patients with strong hair should avoid the hair area (Figure 1a). Further, the photoconductive treatment head is laterally close to the lower eyelid edge for treatment, the light spots are connected and the overlap is no more than 10%, and the operation is performed twice (Fig. 1b). Patients with severe upper eyelid lesions can be treated with a small therapeutic head on the upper eyelid after placing the eye shield (Fig. 1c). (5) after IPL irradiation postprocessing IPL irradiation, facial gel can be cleaned and combined with meibomian gland massage. (6) The treatment cycle is 3 ~ 4 times of IPL treatment as a course of treatment, with an interval of 2 ~ 4 weeks between the two treatments. The single course of treatment is usually 2 ~ 4 months, and the course of treatment can also be extended according to the treatment situation to consolidate the treatment effect.
5. Efficacy and treatment of IPL in the treatment of MGD and its related dry eyes
5.1 therapeutic effect and recommended scheme of MGD and related dry eyes
For ophthalmologists, the treatment of MGD is a challenging task. Although the treatment of MGD includes schemes such as eyelid hot compress and cleaning, it still needs a long-term chronic disease management process. The acceptance rate of IPL treatment in MGD patients gradually increases with the passage of time and the manifestation of treatment effect. More and more studies and clinical practice show that IPL treatment of MGD and its related dry eyes is safe and effective. Clinical studies showed that after IPL treatment, the ocular surface disease index (osdi), tear break-up time (TBUT), eyelid fat quality of meibomian gland, meibomian gland excretion capacity and meibomian gland atrophy were significantly improved, but there were no significant changes in tear secretion and tear osmotic pressure [4]. IPL treatment can significantly improve the clinical symptoms of patients with MGD related dry eyes, reduce related ocular surface inflammation, improve the function of meibomian gland and reconstruct the general structure of meibomian gland. The results of a randomized controlled clinical trial showed that IPL treatment could open the opening of meibomian gland, improve the microstructure of meibomian gland, the maximum diameter of meibomian gland acinus and the unit density of meibomian gland acinus, and the positive rate of inflammatory cells around gland structure decreased significantly [16]. Liu et al. [18] reported the effect of IPL treatment on 44 patients with MGD. The irradiation energy was 14 ~ 16 J / cm2, with an interval of about 4 weeks. The patients were treated for 3 times. After treatment, the levels of inflammatory markers interleukin (IL) - 17a, IL-6 and prostaglandin E2 (PGE2) in the tear film decreased significantly; Other studies showed that the levels of inflammatory factors such as IL-4, IL-6, IL-10 and IL-17A in patients' tears decreased significantly after treatment [19]. These results show the ability of IPL treatment to improve the microstructure of meibomian gland and inhibit the inflammatory response around meibomian gland and ocular surface in patients with MGD [16,20]. It is recommended to treat MGD and its related dry eyes with IPL for 3 ~ 4 times as a course of treatment, and the interval between each two treatments is 2 ~ 4 weeks. During the treatment cycle, patients are recommended to continue hot compress treatment at home and clean the eyelid margin. For example, use 0.01% hypochlorous acid eye wash, and use artificial tears or eye drops to promote tear secretion, Artificial tears containing lipid components are preferred. After one course of IPL treatment, eye surface tear and meibomian gland function should be tested to evaluate the treatment effect. 3 ~ 6 months after the completion of IPL treatment at the end of the course of treatment, the treatment plan can be adjusted or re formulated according to the patient's osdi score and the above test results.
5.2 IPL treatment in patients with refractory MGD
Refractory MGD is defined as those who fail to respond to at least three conventional treatments within at least 2 years, including local or systemic anti-inflammatory treatment, local or systemic antibiotic treatment, moisturizing eye drops or local ointment application, automatic thermal pulsation therapy and tarsal gland catheterization [8,21]. There is increasing evidence that IPL therapy in patients with MGD can help alleviate dry eye symptoms [1,6,8,21-30]. Arita et al. [21] used IPL combined with meibomian gland extrusion therapy for 8 times in patients with refractory MGD who were ineffective in regular hot compress and drug treatment, with an interval of 3 weeks. They evaluated the safety and effectiveness of the treatment and found that this therapy can improve tear film homeostasis and reduce ocular symptoms in patients with refractory MGD, which has a good application prospect. Huang et al. [31] treated patients with refractory obstructive MGD with IPL combined with meibomian gland probing (MGP). The treatment effect was evaluated by dry eye symptom questionnaire score, TBUT, meibomian gland function, improvement of meibomian neovascularization and other indicators. It was found that in the simple IPL treatment group The above indexes of patients in the simple MGP treatment group and the mgp-ipl combined treatment group were significantly improved. Compared with the simple IPL treatment group or the simple MGP treatment group, the signs and symptoms of the mgp-ipl combined treatment group were improved more significantly, and the effect was the best in alleviating the long-term symptoms of patients [31]. It is suggested that patients with refractory MGD can be treated with IPL combined with meibomian gland extrusion, MGP or thermal pulsation, so as to strengthen the therapeutic effect of IPL, and the treatment times of IPL can be increased according to the needs of patients.
5.3 IPL treatment effect and treatment scheme of mite blepharitis
Demodex blepharitis is defined as a chronic inflammatory disease caused by demodex infection of the eyelid margin. The lesions mainly involve the eyelid skin, ciliary sac and meibomian gland. The typical clinical manifestations are eye itching, foreign body sensation, dry eye, eyelid congestion, scale like attachment and cuff secretion at the root of eyelashes. In severe cases, it can cause conjunctival and corneal complications, The main treatments include eyelid cleaning, eye compress and massage, topical application of 0.01% chloric acid eye drops, tea tree oil wet wipes or tea tree oil ointment, metronidazole eye ointment or gel, anti-inflammatory drugs and systemic drugs for treatment of [31-32].
IPL treatment can reduce the number of tarsal mites, improve the subjective symptoms of dry eye patients and objective indicators such as TBUT and corneal fluorescence staining, increase the excretion of lipid secreted by meibomian gland, improve the quality of eyelid fat, and inhibit the formation of meibomian neovascularization [33]. Huo et al. [34] used opt (5th generation IPL Technology) to treat MGD patients with mite infection and MGD patients without mite infection, and compared the treatment effects. The results showed that the two groups had osdi score, conjunctival congestion score, TBUT, corneal staining score, meibomian gland atrophy degree score, meibomian margin morphology abnormality Meibomian gland excretion function and eyelid fat quality score were significantly improved compared with those before treatment. Compared with non Demodex MGD eyes, the improvement of eyelid fat excretion and eyelid fat quality of Demodex infected MGD eyes after IPL treatment was more significant, but the repair speed of corneal epithelial injury was slower. It is suggested that patients with Demodex blepharitis can choose IPL treatment on the basis of local acarid treatment on the blepharal margin. After the course of treatment, the number of meibomian gland mites should be detected, and the function of eye surface tears and meibomian gland should be evaluated.
6. Adverse reactions and prevention of IPL ophthalmic treatment
Ophthalmologists using IPL to treat dry eyes should pay attention to avoid potential adverse reactions. The common adverse reactions of IPL in the treatment of dermatological diseases are local pain and temporary skin flushing, which can disappear automatically 1 ~ 2 hours after treatment. After IPL treatment of dry eyes, local crusting, edema or blisters of the skin are mostly caused by excessive irradiation energy or repeated overlap of light spots. Personalized parameter setting and correct operation can avoid such adverse reactions, and the local edema can subside within 7 days. After treatment, local skin pigmentation or depigmentation mostly occurred in dark skin color or those who were over exposed to sunlight in the treatment area, which can recover automatically after 3 ~ 6 months. Serious eye complications caused by IPL facial treatment recorded by dermatology include uveitis, photophobia and pupil abnormalities. The complications observed by ophthalmology include the onset of trichiasis syndrome, new vitreous opacity or aggravation of original vitreous opacity, which may be related to inadequate eye protection measures [30].
The consensus expert group suggests that eye protection should be done well during dry eye treatment. Patients should naturally close their eyes or look at the top of their head during lower eyelid treatment. Patients are required to close their eyes and look at the direction of their toes during upper eyelid treatment, and an eye shield should be placed at the cornea of the eye to prevent eye tissue damage caused by iris pigment absorbing irradiation energy. During IPL treatment, if the pulse spot is accidentally emitted to the hair growth parts such as eyebrows and eyelashes, resulting in hair absence, the hair growth can be recovered about 1 month after treatment, and one IPL irradiation will not cause permanent hair removal. The consensus expert group suggests that it is forbidden to wash your face with overheated water within 3 days after IPL treatment, and pay attention to sunscreen within 1 month after treatment, so as not to promote the formation of melanin and lead to pigmentation of eyelid skin. The skin that has just received strong sunlight is very sensitive to infrared radiation, so IPL treatment can not be carried out temporarily. IPL treatment should be carried out 3 ~ 4 weeks after strong light exposure. Contraindications for IPL treatment include solar dermatitis, skin malignancy, systemic lupus erythematosus and those who have taken photosensitive drugs in recent 1 month. During the treatment, the operator should emphasize the protection of the eye, avoid the IPL light source from directly irradiating the cornea and intraocular tissues, and pay attention to the condition evaluation of previous eye diseases such as iritis. The IPL strong light should avoid the hair growth parts such as eyelashes and eyebrows. In addition, the pigmented plaque around the eye and the existing skin lesions should also be fully evaluated.
Since MGD related dry eye is a chronic disease that cannot be cured, and most of the follow-up time of IPL treatment of eye diseases so far is no more than 1 year, we should pay attention to follow-up and observe the long-term efficacy of IPL treatment of MGD related dry eye. At present, the clinical frequency of IPL treatment of MGD related dry eyes varies greatly, ranging from 2 to 12 times. There is no unified requirement for the follow-up time. At present, it is mostly 3 to 12 months, and there are also great differences. Therefore, the best scheme of IPL treatment frequency, treatment duration and follow-up time still needs to be further explored and evaluated. Considering the long-term challenge of MGD treatment, trying to use a variety of methods may be beneficial to the treatment of MGD. At the same time, we should explore the best combination mode of a variety of physical therapies, including but not limited to emphasizing tarsal margin cleaning, combined IPL and meibomian gland massage, meibomian gland exploration or thermal pulsation, which will help to further promote the clinical application of IPL. The standardization of IPL on MGD and its related dry eye treatment scheme is helpful to better carry out relevant clinical research to explore the effects of gender, age and other factors on IPL treatment response. In addition, it will help to develop a consensus on the treatment of MGD and its potential value.
It is stated that this article is only an expert opinion and provides guidance for clinical medical services, not a medical standard that must be followed in all cases; The content of this article has no economic interest with the manufacturers of related products
Members of the consensus forming expert group:
Writing expert:
Hong Jiaxu eye, ear, nose and Throat Hospital Affiliated to Fudan University
Huang Xiaodan Second Affiliated Hospital of Medical College of Zhejiang University
Jin Xiuming Second Affiliated Hospital of Medical College of Zhejiang University
Members of the expert group (in alphabetical order of last name, regardless of order):
Chen Baihua Xiangya Second Hospital of Central South University
Chen Jili Shanghai Shibei hospital
Chen Luxia Tianjin ophthalmic hospital
Chen Qi Guangxi Autonomous Region People's Hospital
Chen Wei, optometry Hospital Affiliated to Wenzhou Medical University
Ding Lin people's Hospital of Xinjiang Uygur Autonomous Region
Dong Nuo Xiamen ophthalmology center affiliated to Xiamen University
Feng Yun Third Hospital of Peking University
Fu Yao Ninth People's Hospital Affiliated to Medical College of Shanghai Jiaotong University
Gaohua Shandong ophthalmic hospital
Gu Hao Affiliated Hospital of Guizhou Medical University
Gu Zhengyu the First Affiliated Hospital of Anhui Medical University
Jiang Jing Eye Hospital of Nanjing Medical University
Ke Bilian first people's Hospital Affiliated to Shanghai Jiaotong University
Li Guigang Tongji Hospital Affiliated to Tongji Medical College of Huazhong University of science and technology
Li Lan Kunming first people's Hospital
Li Lin Affiliated Hospital of Inner Mongolia Medical University
Li Ying Xi'an fourth hospital
LongQin Peking Union Medical College Hospital
Qu Jifang Shanghai Children's Medical Center affiliated to Medical College of Shanghai Jiaotong University
Wang Linnong Nanjing First Hospital
Wu Juan Xining first people's Hospital
Wu Pengcheng Second Hospital of Lanzhou University
Xiao Xianghua Xi'an First Hospital
Xie Huatao Wuhan Union Medical College Hospital
Xu Mei the First Affiliated Hospital of Chongqing Medical University
Yang Yanning people's Hospital of Wuhan University
Yuman Sichuan Provincial People's Hospital
Zeng Qingyan Wuhan Aier Eye Hospital Hankou hospital
Zhang Lijun Dalian Third People's Hospital
References (omitted)